Dr. Patrick White, Chief of Palliative Medicine and Professor of Medicine, delivered a presentation titled “Designing a Better Care Experience: Facilitating Patient-Directed Transitions of Care at End-of-Life” during Grand Rounds at the Centers for Medicare & Medicaid Services (CMS) on December 3, 2025. Please find his presentation linked below.
Page index: Our Challenge: Late Transitions | Factors Contributing to Late Transitions of Care | Our Solution: Designing a Novel Multifaceted Intervention | Outcomes of the Targeted Goals of Care Initiative (TGI) | Program Impact: Palliative Care Encounters | Program Impact: Inpatient Hospice Growth | Opportunity to Enhance Patient-Directed Transitions of Care #1 | Opportunity to Enhance Patient-Directed Transitions of Care #2 | Opportunity to Enhance Patient-Directed Transitions of Care #3 | Conclusion

Designing a Better Care Experience: Facilitating Patient-Directed Transitions of Care at End-of-Life
- Our Challenge
- Hospice transitions often occur late reducing the potential benefit
- Too many Americans with terminal illness spend time in the ICU during the last few months of life.
- Our Solution
- Multifaceted Intervention using AI
- Enhancing provider communication skills
- Hybrid ICU support model
- Remaining Opportunities
- Developing more contemporary hospice diagnoses
- Opportunity for enhanced support in the home
- Realizing the potential of time-limited concurrent care

Our Challenge: Late Transitions
- Hospice care is associated with increased family caregiver perception of high-quality end-of-life care
- While the Medicare Hospice Benefit was designed as a 6-month benefit, US median hospice length of stay is currently only 18 days
- Despite this 50.9% of Medicare decedents did not receive ANY hospice care.
Wright AA, Keating NL, Ayanian JZ, Chrischilles EA, et al. Family Perspectives on Aggressive Cancer Care Near the End of Life. JAMA. 2016 19;315(3):284-92.
2024 Edition: Hospice Facts and Figures. Alexandria, VA: National Alliance for Care at Home.
Factors Contributing to Late Transitions of Care
- Health care systems struggle to identify high mortality risk patients
- Clinicians may lack the skills, time, and/or incentives to provide patients with critical prognostic information
- Patients in the ICU require a significant amount of supportive care to transfer out which is currently less incentivized
Our Solution: Designing a Novel Multifaceted Intervention
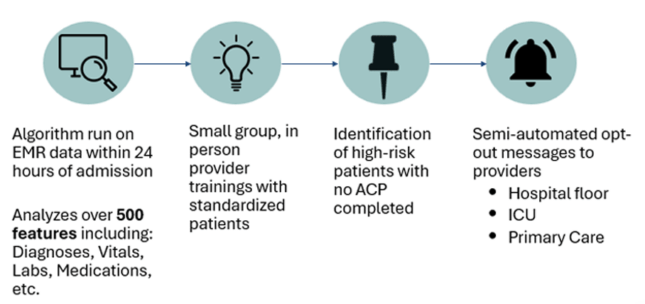
Outcomes of the Targeted Goals of Care Initiative (TGI)
| Control | TGI | P-value | |
|---|---|---|---|
| Informal Goals of Care/ACP Discussion | 14% | 58% | <0.001 |
| Formal Goals of Care/ACP Note | 3% | 23% | <0.001 |
| Time to Goals of Care Discussion | 5.84 days | 3.07 days | <0.001 |
| Discharge Code Status | Control | TGI Group | P-value |
|---|---|---|---|
| Full Code | 92% | 80% | <0.001 |
| Comfort Care Only | 2% | 3% | |
| Limited Code | 6% | 17% |
Chi S, Kim S, Reuter M, Ponzillo K, Oliver DP, Foraker R, Heard K, Liu J, Pitzer K, White P, Moore N. Advanced Care Planning for Hospitalized Patients Following Clinician Notification of Patient Mortality by a Machine Learning Algorithm. JAMA Netw Open. 2023;6(4):e238795.
Program Impact: Palliative Care Encounters
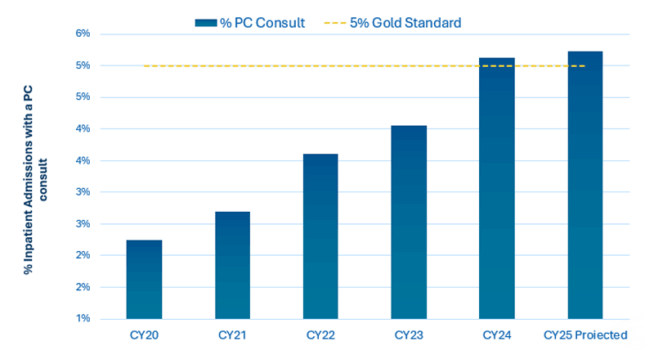
Data source: Palliative Care Dashboard in Power BI
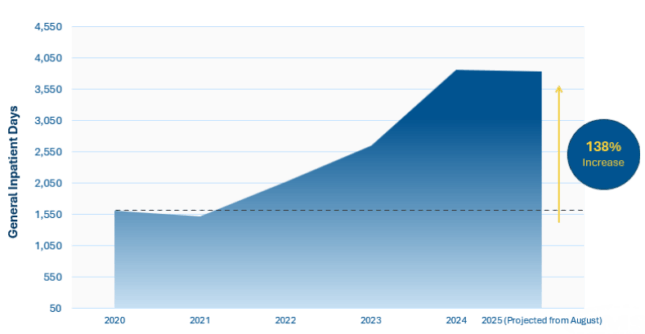
Program Impact: Inpatient Hospice Growth

Opportunity to Enhance Patient-Directed Transitions of Care #1: More Holistic Hospice Eligibility Criteria
- LCD hospice eligibility guidelines over-emphasize a single hospice diagnosis.
- Mortality in the U.S. has been increasingly driven by multiple comorbid conditions.
- A more holistic prognostication approach is needed with training of key parties
- MACs, QICs, ALJs, etc.
Washington K, Lewis A, Foraker R, White P, et al. Accuracy of Medicare Hospice Local Coverage Determination Guidelines for End-Stage Kidney Disease. Journal of Palliative Medicine. in Press.
Opportunity to Enhance Patient-Directed Transitions of Care #2: Enhancing Support in the Home by Improving Continuous Care
- Many patients wish to be at home in their final days but a lack of support in the home results in inpatient deaths.
- Continuous care is associated with a 71% reduction in the odds of dying in the inpatient setting, helping patients to die at home, and an 80% reduction in hospice disenrollment.
- Current regulations require 8 hours of care be delivered in a calendar day (midnight to midnight) which limits its practicality and use.
- Increasing the flexibility of the benefit to 8 hours of continuous care within any 24-hour period, will significantly increase utilization of this valuable benefit.
Casarett D, Harrold J, Harris PS, Bender L, Farrington S, Smither E, Ache K, Teno J. Does Continuous Hospice Care Help Patients Remain at Home? J Pain Symptom Manage. 2015;50(3):297-304.
Opportunity to Enhance Patient-Directed Transitions of Care #3: Time-limited Concurrent Care
- Concurrent care allows the simultaneous delivery of hospice care while still providing complex medical care (e.g. chemotherapy, hemodialysis, etc.)
- It demonstrates potential to act as a bridge to hospice and facilitate earlier transitions of care.
- Many potential models of concurrent care have been trialed with varying degrees of success
- In veterans with advanced lung cancer concurrent care has been associated with:
- Reduced aggressive interventions (AOR 0.66)
- Reduced ICU use (AOR 0.78)
- Reduced cost ($266 per day lower cost)
- No change in overall survival
- Optimal patient populations, timing, and hospice reimbursement requires further research but appreciate CMMI efforts!
Mor V, Wagner TH, Levy C, Ersek M, Miller SC, Gidwani-Marszowski R, Joyce N, Faricy-Anderson K, Corneau EA, Lorenz K, Kinosian B, Shreve S. Association of Expanded VA Hospice Care With Aggressive Care and Cost for Veterans With Advanced Lung Cancer. JAMA Oncol. 2019;5(6):810-816.
Conclusion
- We can design a better care experience at end of life by utilizing a multifaceted intervention to identify high mortality risk patients, improve provider training, and enhance support for ICU patients.
- Key regulatory enhancements could include promoting more holistic hospice eligibility criteria, increasing the flexibility surrounding continuous care, and continuing to develop an ideal time-limited concurrent care model.
- This work has been significantly aided by the CMS Age-Friendly Measures specifically Eliciting Patient Healthcare Goals.
- These initiatives have the potential to decrease inpatient deaths, enhance the patient and caregiver experience, and reduce the total cost of care.